Should psoriasis patients continue biologics during the COVID-19 pandemic? Plus CMS implements changes to aid the COVID-19 response
- Af
- Episode
- 43
- Published
- 2. apr. 2020
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 43 of 100
- Længde
- 12M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
Patients with severe psoriasis may be at higher risk for infection because of increased inflammation in the body. Dr. Lawrence Green discusses how to counsel patients who are taking biologics to control their psoriasis during the COVID-19 pandemic. "What I recommend [is to] stay on your biologic as long as you can unless you have exposure [or] you start to feel feverish," Dr. Green advises. * * * We also bring you the latest in dermatology news and research: 1. CMS implements temporary regulatory changes to aid COVID-19 response 2. FDA issues EUA allowing hydroxychloroquine sulfate, chloroquine phosphate treatment in COVID-19 3. FDA okays emergency use of convalescent plasma for seriously ill COVID-19 patients 4. Physician couples draft wills, face tough questions amid COVID-19 * * * Key takeaways from this episode: • Patients with uncontrolled psoriasis symptoms are at higher risk for developing infection and other comorbidities. "In general, I have told patients that if they stop the biologic for some time and the psoriasis comes back so that it's severe again, I think that it's significantly more risky for getting COVID-19 than if they continue to take their biologic," says Dr. Green. • There currently are no data on whether biologics help or harm patients with COVID-19. • Anti–tumor necrosis factor (anti-TNF) agents may be useful in helping control pneumonia, but they also are associated with an increased risk for infection, compared with other biologic agents. It may be safer for patients to switch to or continue treatment with anti–IL-17 or anti–IL-23 agents during the COVID-19 pandemic. • Patients should stop biologic treatment if they have exposure to someone with COVID-19 or start to show symptoms. "Stopping a biologic for a few weeks will not bring your psoriasis back. ... [but] a few months off can make a difference," Dr. Green explains. • Patients currently on biologics should take extra precautions to practice social distancing, stay at home when possible, wash hands, use hand sanitizer, and avoid touching the face, as recommended by the Centers for Disease Control and Prevention. • For additional resources, dermatologists can consult the American Academy of Dermatology • or the National Psoriasis Foundation • guidelines on psoriasis treatment during the COVID-19 pandemic. * * * Host: Nick Andrews Guest: Lawrence J. Green, MD (George Washington University, Washington) Show notes by: Alicia Sonners, Melissa Sears * * * You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
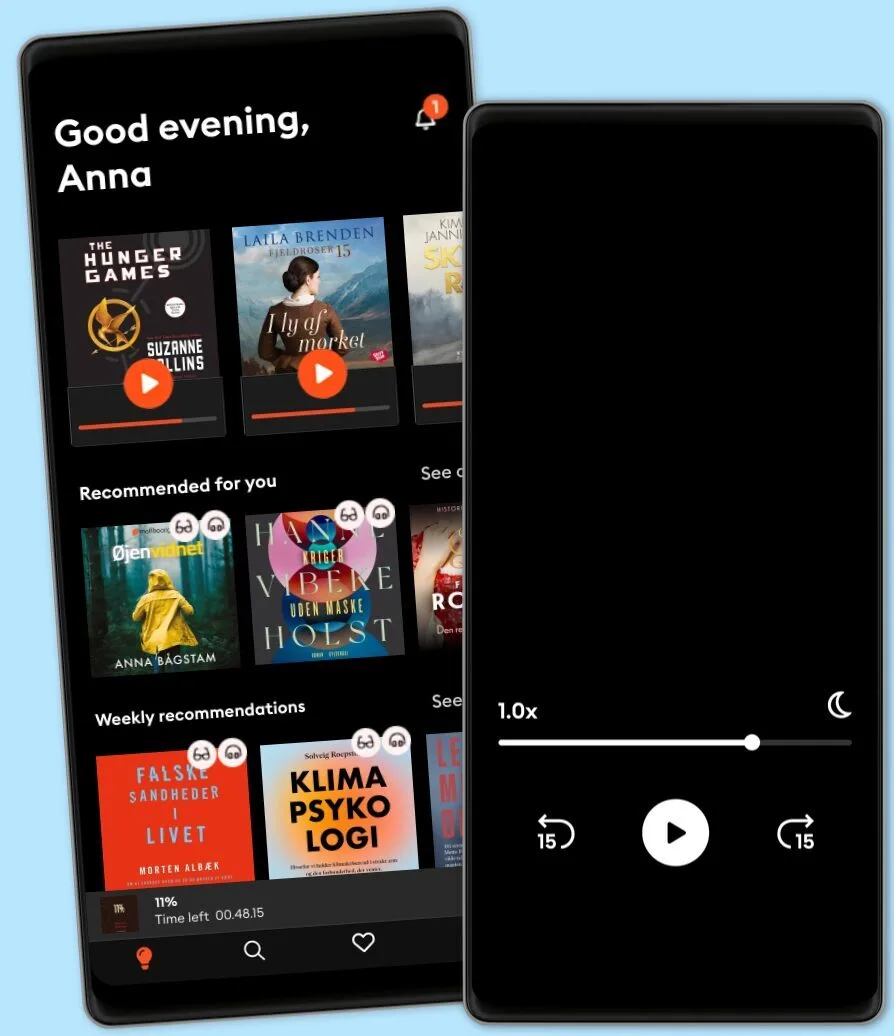
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark