Resident Takeover: Prescribing combined OCs; contact dermatitis tips; fetal isotretinoin exposure
- Af
- Episode
- 6
- Published
- 25. jul. 2019
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 6 of 100
- Længde
- 29M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
Combined oral contraceptives (COCs) have many uses in dermatology, but dermatologists often underutilize COCs and don't feel comfortable prescribing them. In this special resident takeover of the podcast, three dermatology residents — Dr. Daniel Mazori, Dr. Elisabeth Tracey, and Dr. Julie Croley — review the basics of prescribing COCs for dermatologic conditions. Beginning at 8:36, they discuss assessment of patient eligibility and selection of COCs, proper use of COCs, and management of risks and side effects. We also bring you the latest in dermatology news and research: 1. iPledge: Fetal exposure to isotretinoin continues Although pregnancy-related adverse events have decreased, pregnancies, abortions, and fetal defects associated with isotretinoin exposure continue to be a problem. 2. Expert shares contact dermatitis trends Dr. Rajani Katta talks about what's happening in contact dermatitis, including an uptick in allergic reactions to essential oils contained in "all natural" products. Things you will learn in this episode: • Acne is the main indication for COCs in dermatology, but other off-label uses include hidradenitis suppurativa, hirsutism, female pattern hair loss, and autoimmune progesterone dermatitis. • When prescribing COCs, it is important to consider absolute and relative contraindications such as cardiovascular disease, postpartum status, women 35 years and older and smoking more than 15 cigarettes per day, migraine with aura, and history of diabetes for more than 20 years, plus others. • Rule out pregnancy prior to starting COCs via a urine or serum pregnancy test. Dr. Croley points out, "A pelvic exam is not required to start combined oral contraceptives, as is sometimes thought by providers." • Monophasic formulations are considered first-line therapy. • For patients who are concerned about symptoms associated with a hormone-free interval during treatment, choose a COC that does not include placebo pills, or encourage the patient to skip the placebo pills altogether and start the next pack earlier. • Estrogen-related side effects are a consideration when prescribing COCs. "In general, the lowest possible dose of estrogen that is effective and tolerable should be prescribed," Dr. Libby advises. • Combined oral contraceptives can be started on any day of the patient's menstrual cycle, but patients should be counseled to use backup contraception for 7 days if the COC is started more than 5 days after the first day of their most recent period. • At least 3 months of therapy can be expected to evaluate the effectiveness of COCs for acne, potentially up to 6 months. • Breakthrough bleeding is the most common side effect of COCs and can be minimized by taking the COC at about the same time every day and avoiding missed pills. If breakthrough bleeding persists after 3 cycles, consider increasing the estrogen dose or referring the patient to an obstetrician/gynecologist. • Discuss the risk of venous thromboembolism with patients using the 3-6-9-12 model • . Hosts: Elizabeth Mechcatie, Terry Rudd Guests: Daniel R. Mazori, MD (State University of New York Downstate Medical Center, Brooklyn); Elisabeth "Libby" Tracey, MD (Cleveland Clinic Foundation, Ohio); Julie Ann Amthor Croley, MD (The University of Texas Medical Branch at Galveston). Show notes by Alicia Sonners, Melissa Sears, and Elizabeth Mechcatie. You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
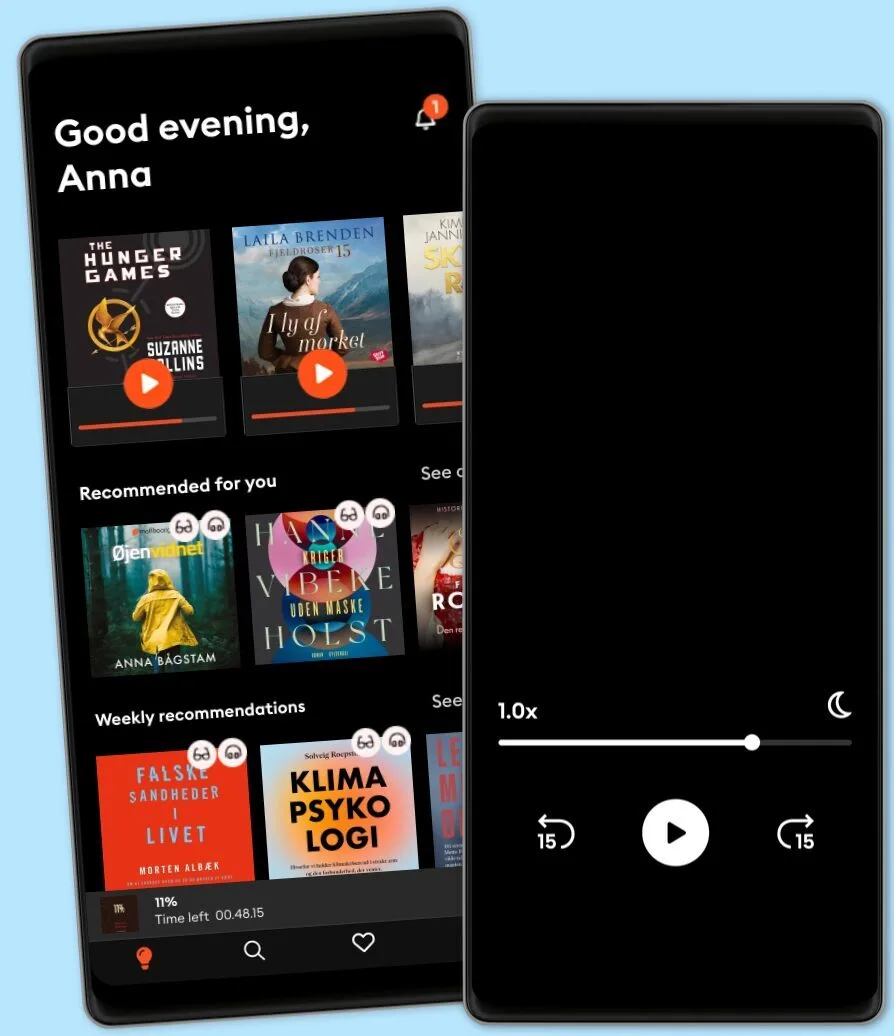
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark