Ocular chemical injuries in the dermatology office, plus social media and cosmetic surgery, and moving from psoriasis to psoriatic arthritis
- Af
- Episode
- 3
- Published
- 4. jul. 2019
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 3 of 100
- Længde
- 30M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
Are you and your staff prepared to handle ocular chemical injuries? Dr. Vincent DeLeo talks with Dr. Shawna K. Langley and Dr. Deborah Moon about common chemical agents used in the dermatology office that can be damaging to the eyes. Dr. Langley shares her experience with a patient who sustained a transient ocular injury following accidental exposure to aluminum chloride during a biopsy of a suspicious lesion on the cheek. Treatment protocols and prevention methods that dermatologists can implement to ensure the best outcome for patients also are discussed. We also bring you the latest in dermatology news and research: 1: Infections linked with transition to psoriatic arthritis 2: Social media use linked to acceptance of cosmetic surgery 3: Severity, itch improvements remain steady with ruxolitinib for atopic dermatitis Things you will learn in this episode: • On average, approximately 7%-10% of all ocular traumas may be attributed to chemical burns. • The two most important factors to consider when evaluating the extent of an ocular chemical injury include the properties of the chemical and the duration of exposure. • Damage associated with exposure to acidic chemicals usually is limited to more superficial consequences, while exposure to alkaline chemicals can result in more serious long-term effects such as cataracts or glaucoma caused by deeper penetration of the eye structures. • The most common immediate side effects of ocular chemical injuries include a sensation of burning (not necessarily immediate) or pain as well as redness or erythema of the eye and eventually vision changes. "One of the learning points to me was that if somebody complains that something has dripped in their eye, even if it doesn't seem possible and it doesn't really make sense, and if you had just worked with a caustic substance right before they said that, have them start flushing immediately anyway," said Dr. Langley. • The Roper-Hall classification • outlines the prognosis based on grade of injury (grades I-IV). • Immediate irrigation of the eye for 15-30 minutes is the most important variable, which will affect the patient's long-term prognosis. "This is the one variable that will impact the long-term outcome the most for the patient," said Dr. Langley. • Always ask patients if they are wearing contact lenses, as chemicals trapped underneath can cause prolonged burning of the eye. Do not delay irrigation to remove contact lenses. Start irrigation immediately and remove the lenses when possible under irrigation. • Emphasize urgent follow-up with an ophthalmologist following ocular chemical injuries sustained in the dermatology office. If an ophthalmologist is not immediately available, send the patient to the emergency department. • Educate support staff about the potential for ocular injuries in the dermatology office and be prepared with the proper equipment to administer immediate treatment. Hosts: Elizabeth Mechcatie; Terry Rudd; Vincent A. DeLeo, MD (Keck School of Medicine of the University of Southern California, Los Angeles) Guests: Shawna K. Langley, MD (Loma Linda [Calif.] University Medical Center; Deborah J. Moon, MD (Kaiser Permanente Los Angeles [Calif.] Medical Center and the University of California, Irvine) Show notes by: Alicia Sonners, Melissa Sears, Elizabeth Mechcatie You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
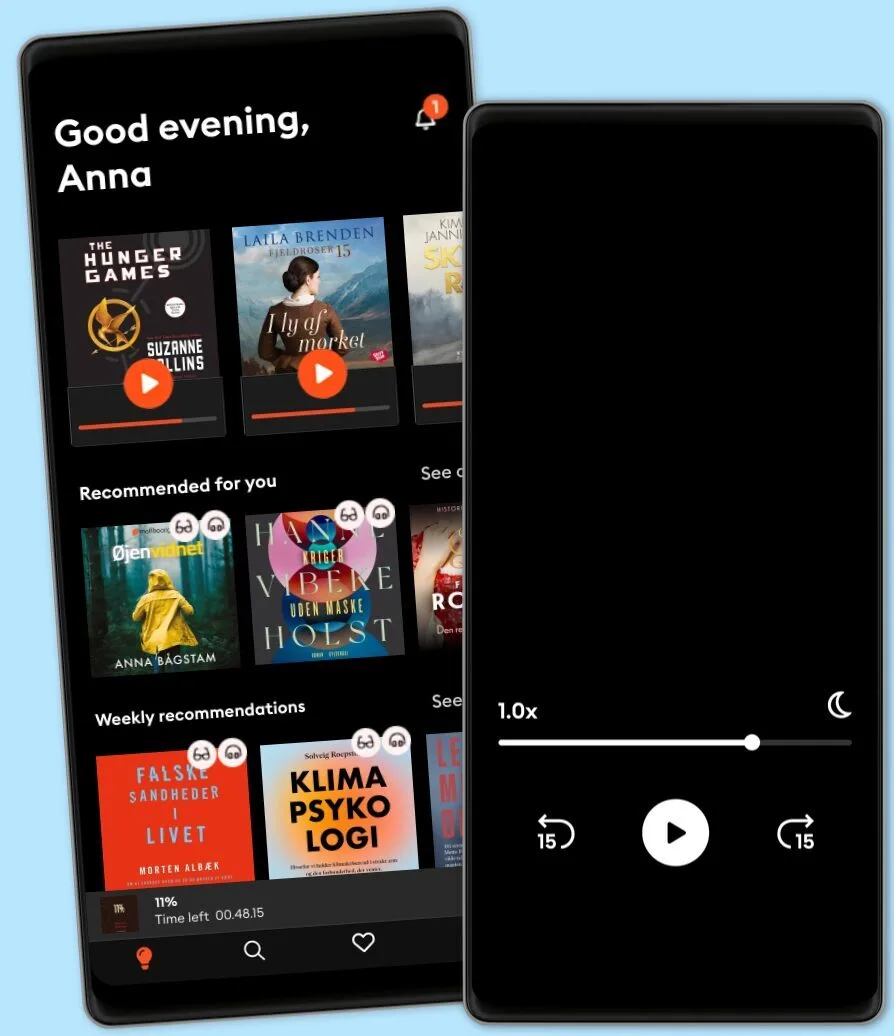
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark