Hyperbaric oxygen therapy in dermatology, plus nemolizumab tames itching in prurigo nodularis patients
- Af
- Episode
- 39
- Published
- 5. mar. 2020
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 39 of 100
- Længde
- 25M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
Hyperbaric oxygen therapy (HOT) is an effective second-line treatment option anytime there is a chronic complicated wound or tissue with vascular compromise. Dr. Josephine Nguyen, president of the Association of Military Dermatologists, talks with Dr. Emily Wong and Dr. Jonathan Jeter about how dermatologists can use HOT. "The most common scenario ... would be a situation where you have a compromised flap or graft after a surgery," says Dr. Jeter "[The site is] not getting enough blood flow that's threatening it to necrose ... hyperbaric oxygen therapy can come in [and] can increase the oxygen delivery to those sites," says Dr. Jeter. They discuss the mechanism of action for HOT, tips for treatment, and potential complications. * * * We also bring you the latest in dermatology news and research: 1. What medical conferences are being canceled by coronavirus? Despite COVID-19, most U.S. medical conferences are moving forward as planned. 2. Nemolizumab tames itching in prurigo nodularis patients in phase 2 study Adults with moderate to severe prurigo nodularis who were treated with the investigational drug nemolizumab showed significant improvement in itching, compared with patients who received placebo. 3. Esophageal stricture signals urgent treatment in kids with butterfly skin A quarter of urgent contacts in 20 children with generalized severe recessive dystrophic epidermolysis bullosa were tied to esophageal narrowing. * * * Things you will learn in this episode: • Hyperbaric oxygen therapy is best known for treating decompression sickness (e.g., "the bends" in scuba divers or aircrew members) and carbon monoxide poisoning. "[HOT] occurs in a specialized chamber that gradually becomes pressurized in order to increase the ambient pressure," Dr. Wong explains. "Then the pressure can return to atmospheric pressure in a controlled, slow manner." • In addition to persistent wounds and compromised grafts and flaps, other dermatologic applications for HOT include radiation-induced ulceration, vasculitis/vasculopathy, and autoimmune reactions. • Patients may inquire about HOT for anti-inflammatory conditions such as psoriasis, but there currently is no evidence to support its effectiveness. Only published dermatologic indications for HOT are recommended until more research is conducted. • According to the Undersea & Hyperbaric Medical Society • , there currently are nearly 200 accredited HOT locations in the United States. Hyperbaric oxygen therapy is most likely to be available within large medical centers and is less common in rural areas. • In cases in which tissue is threatened, it is important to refer patients for HOT sooner rather than later. "The longer it goes since the initial injury or loss of blood flow, the less likely [HOT is] going to be effective," notes Dr. Jeter. • Dermatologists typically need to refer patients to large academic medical centers with wound care centers to receive HOT. • Potential complications of HOT include fire, middle ear barotrauma, and reversible myopathy. More severe but rare complications include central nervous system symptoms, seizures, and pulmonary toxicity. • The only absolute contraindication for HOT is an untreated pneumothorax. • Treatment sessions can last anywhere from a few minutes up to several hours. "The longer [the sessions] get, the more likely you are to have complications, but generally around an hour to an hour and a half is a pretty reasonable time period," Dr. Jeter recommends. • In a hyperbaric oxygen chamber, the patient sits or lays down and breathes in pressurized 100% oxygen through a mask or a tight-fitting hood, and the affected skin stays covered with a bandage or the patient's clothing. "Ultimately, it is the increased level of systemic oxygen that promotes wound healing and graft or flap survival. The systemic oxygen improves the fibroblast function, blood flow, vascularity, and mitigates the ischemia-reperfusion injury," explains Dr. Wong. * * * Hosts: Nick Andrews; Josephine Nguyen, MD Guests: Emily B. Wong, MD; Jonathan P. Jeter, MD (San Antonio Uniformed Services Health Education Consortium, Joint Base San Antonio–Lackland, Tex.) Show notes by: Alicia Sonners, Melissa Sears, Elizabeth Mechcatie * * * You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
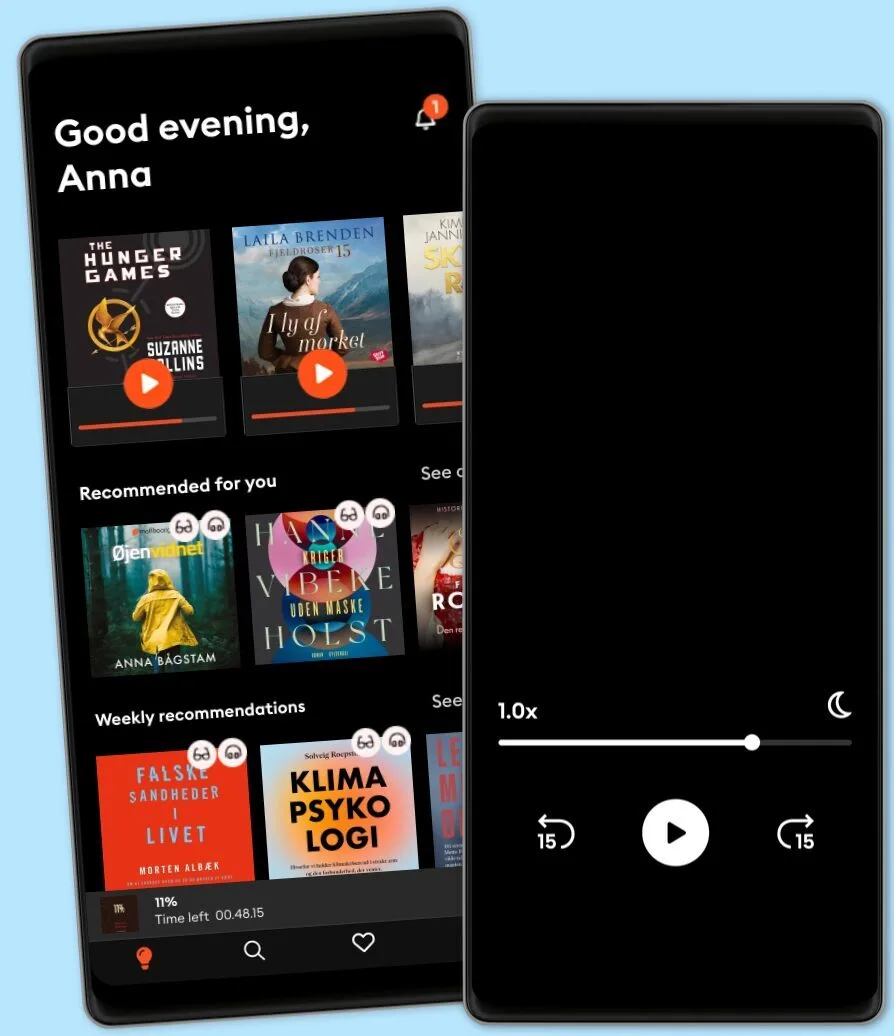
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark