COVID-19: What Dermatologists should know, plus how to use the Fitzpatrick skin type classification?
- Af
- Episode
- 41
- Published
- 18. mar. 2020
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 41 of 100
- Længde
- 25M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
The Fitzpatrick skin type (FST) often is used as a proxy for constitutive skin color, which can lead to confusion. Dr. DeLeo speaks with Dr. Susan Taylor and her colleagues Olivia Ware and Jessica Dawson about the racial limitations of FST in clinical practice. They discuss other classification systems for assessment of skin type and highlight the challenges of creating one system to classify an infinite number of skin tones. * * * We also bring you the latest in dermatology news and research: 1. Paper from Wuhan on dermatology and coronavirus 2. Patients accept artificial intelligence in skin cancer screening 3. Dermatologists best at finding work satisfaction in the office * * * Things you will learn in this episode: • In its early stages, the Fitzpatrick scale was designed to guide dosage for patients undergoing phototherapy by determining who burned and who tanned on exposure to UV light. The Fitzpatrick skin type • has been incorrectly associated with visual stereotypical skin color cues, most likely because there is no other widely adopted classification system for skin color that can be applied to all skin. • In clinical practice, many providers inappropriately use the FST to describe patients' constitutive skin color or race/ethnicity rather than their propensity to burn. • The FST is automatically included in the physical examination portion of many standardized note templates, even for patients without phototherapy needs. • Providers who do not identify as having skin of color may be more likely to use FST to describe constitutive skin color, compared with providers with skin of color. • A more detailed and diverse system to describe constitutive skin color in clinical practice is needed. "The world is becoming so diverse, and there are so many different hues, races, ethnicities, and as dermatologists in the forefront we need to be able to identify pigmentary disorders, identify who will have adverse reactions to a variety of procedures, and thinking about how to do that is really the first step in accomplishing our goal," explains Dr. Taylor. * * * Hosts: Nick Andrews; Vincent A. DeLeo, MD (University of Southern California, Los Angeles) Guests: Susan C. Taylor, MD (University of Pennsylvania, Philadelphia); Olivia R. Ware (Howard University, Washington); Jessica E. Dawson (University of Washington, Seattle) Show notes by: Alicia Sonners, Melissa Sears, Elizabeth Mechcatie * * * You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
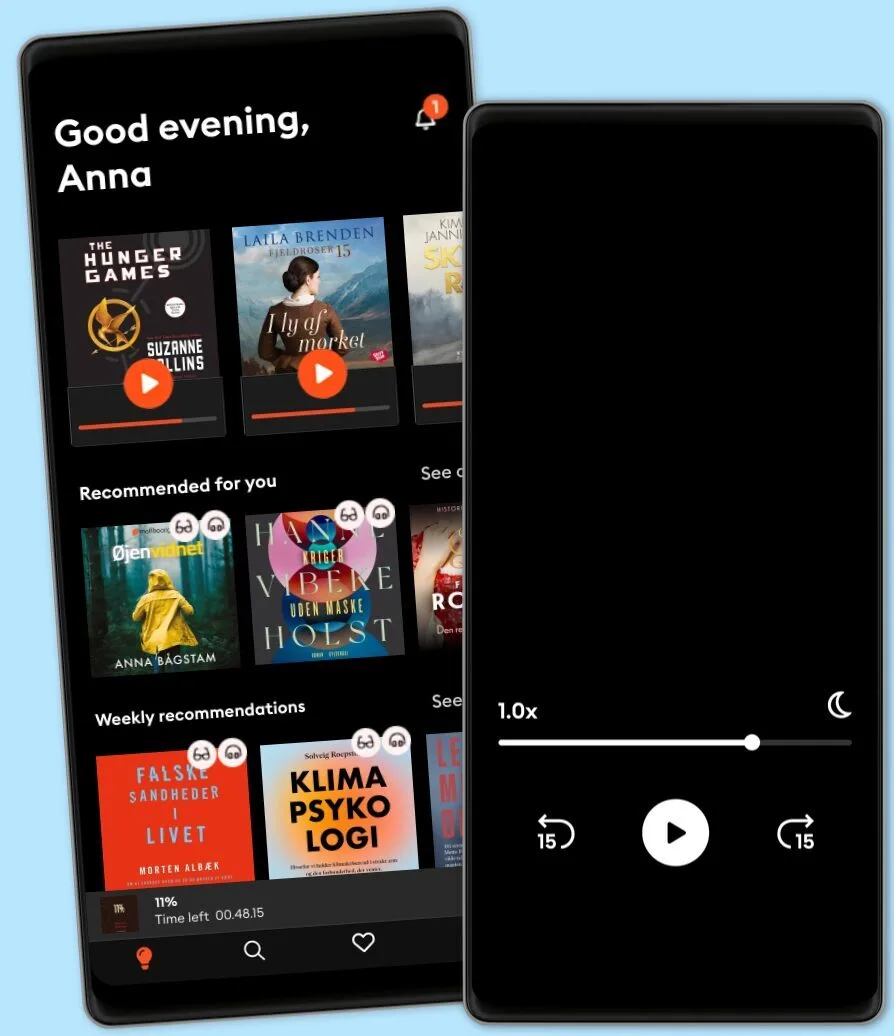
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark