Tools to aid in clinical decision making; plus safety data for tacrolimus; results of a phase 3 study of an IL-17A inhibitor; and clinician burnout.
- Af
- Episode
- 21
- Published
- 31. okt. 2019
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 21 of 100
- Længde
- 27M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
How can you integrate decision-making resources into your clinical practice? In this resident takeover of the podcast, three dermatology residents — Dr. Daniel Mazori, Dr. Elisabeth Tracey, and Dr. Julie Croley — discuss clinical decision support tools such as scoring systems and other resources available for dermatologists. These tools should be used as a supplement, not as a substitute for one's clinical judgment. "The optimal treatment for patients in a complex medical system requires not just coming to the correct diagnosis and using your clinical judgment to make a decision but effectively communicating that decision to the insurance companies [and] to the primary team that's taking care of them on the inpatient service. ... Some objective data can really be useful in those situations," advises Dr. Tracey. * * * Help us make this podcast better! Please take our short listener survey: https://www.surveymonkey.com/r/podcastsurveyOct2019 * * * We bring you the latest in dermatology news and research: 1. No tacrolimus/cancer link in atopic dermatitis in 10-year study 2. PASI-75 with ixekizumab approaches 90% in pediatric psoriasis study 3. NAM offers recommendations to fight clinician burnout * * * Things you will learn in this episode: • Evaluate for psoriatic arthritis with the Psoriasis Epidemiology Screening Tool ( PEST • ). "It's the kind of thing that I'll use in addition to asking a patient with psoriasis questions about symptoms like joint pain and morning stiffness," Dr. Mazori says. • Consider UpToDate.com • and VisualDx.com • for clinical decision support, to formulate differential diagnoses, and as a resource for patient education. "The other day, I had a patient who was diagnosed with scabies," Dr. Tracey explains. "We were counseling the patient on how to decontaminate their environment. I wanted to get the exact number of hours their belongings needed to be in a plastic bag or how to wash their clothes. So, we went on UpToDate and read it together in the clinic." • The SCORTEN system • predicts hospital mortality from Stevens-Johnson syndrome/toxic epidermal necrolysis and is useful for the primary team. "I've found it useful ... as a measure of risk to communicate to the primary team, even the patient's family," Dr. Mazori says. But the SCORTEN isn't perfect. "There are studies that have found it can overestimate or underestimate mortality," he warns. • To differentiate cellulitis from pseudocellulitis in adult patients, consider the ALT-70 score • . "It gives me an objective measure of risk to communicate to the primary team in support of one diagnosis or another in addition to my clinical judgment," advises Dr. Mazori. • The Mohs Appropriate Use Criteria ( AUC • ) helps guide decision making for Mohs micrographic surgery, but it has been scrutinized for classifying most primary superficial basal cell carcinomas as appropriate for treatment, omitting important European trials, and for having ratings that are based on expert opinion rather than evidence. • The MyDermPath+ app • can assist clinicians in forming differentials based on histopathologic patterns. Hosts: Elizabeth Mechcatie, Terry Rudd Guests: Daniel R. Mazori, MD (State University of New York Downstate Medical Center); Elisabeth (Libby) Tracey, MD (Cleveland Clinic Foundation); Julie Ann Amthor Croley, MD (University of Texas Medical Branch at Galveston) Show notes by: Jason Orszt, Melissa Sears, Elizabeth Mechcatie For more MDedge Podcasts, go to mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
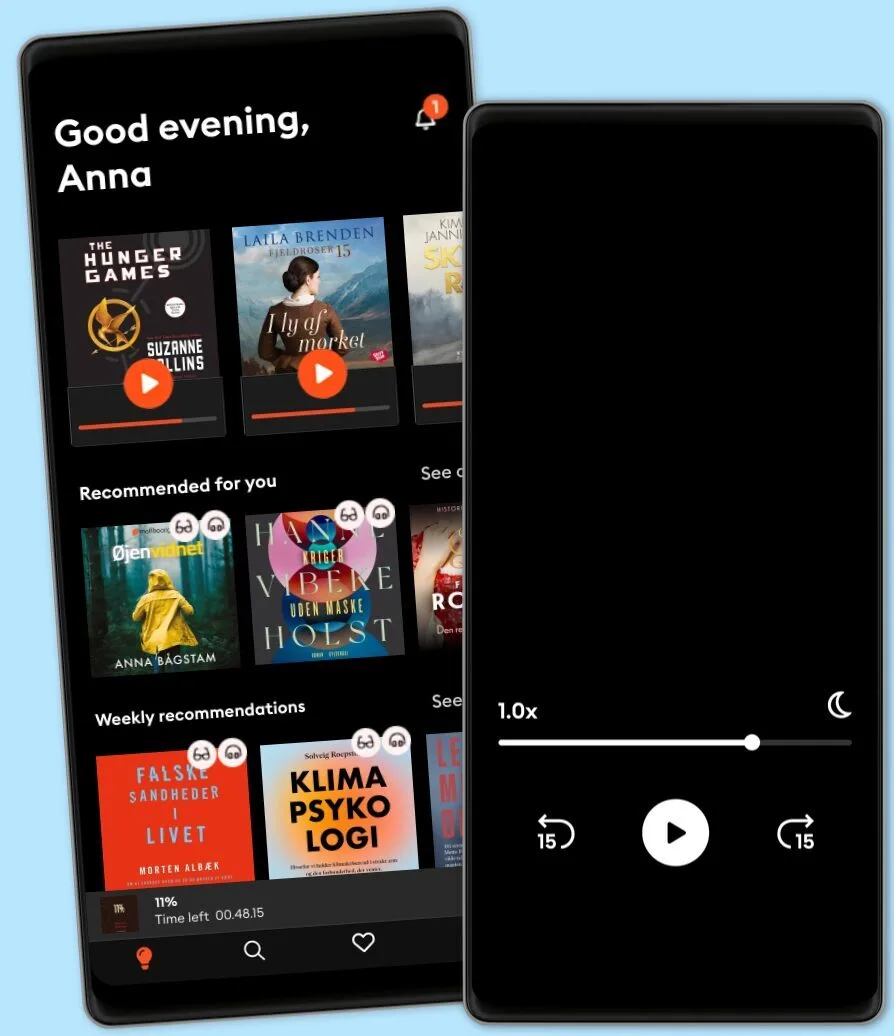
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark