Teledermatology during the COVID-19 pandemic and beyond
- Af
- Episode
- 50
- Published
- 14. maj 2020
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 50 of 100
- Længde
- 36M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
How is dermatology handling this change in practice toward telehealth? Guest host Dr. Candrice Heath talks with Dr. George Han about how dermatologists can adapt their clinical practice to conduct quality teledermatology visits with their patients. "Last year ... I think overall in the health system we probably had about 2,000-3,000 telehealth visits ... by the end of March [this year], I think the numbers I saw [were] around 30,000, so it's absolutely just kind of been a huge change in the way we practice medicine," Dr. Han explained. They discuss potential use cases for teledermatology during the current health crisis and beyond as well as how to address technological barriers to care. * * * We also bring you the latest in dermatology news and research: 1. Novel inflammatory syndrome in children possibly linked to COVID-19 2. Case reports illustrate heterogeneity of skin manifestations in COVID patients 3. COVID-19 Dermatology Registry * * * Things you will learn in this episode: Despite recent HIPAA relaxations, dermatologists still should be aware of privacy and security issues when conducting telehealth visits with patients. Existing resources -- such as noninvasive tests that can be self-administered by patients -- may be useful for concerning lesions that are difficult to diagnose during video visits. "There's this genomic test for melanoma. ... I hadn't used it very much before the COVID pandemic because we could biopsy patients in the office. ... But now that the whole paradigm has changed, I've actually used it more than I ever did before," Dr. Han explained. Common conditions such as psoriasis, acne, and eczema are relatively easy to triage via telemedicine. "We're going to have to do a lot more experimentation, certainly, if there's a lesion that's scaly and erythematous. ... But I think as long as you're up front with the patients, they understand it, too," Dr. Han said. In most cases, total-body skin examinations and evaluation of pigmented or potentially cancerous lesions still warrant an in-person visit. Biologics often can be started in patients with psoriasis or atopic dermatitis without first seeing them in person. "If it's a pretty clear case of psoriasis, I would say that your treatment options are not limited by the fact that we're handling over telemedicine, and I think that's really nice for our patients. There are a number of treatments out there that you don't need laboratory screening for, so those are helpful to have on hand," Dr. Han said. For older patients who may not have the necessary technology skills or devices to participate in video consultations, the Centers for Medicare & Medicaid Services recently issued a guidance that telephone visits will now be paid at the level of an established visit (levels 2–4). "The recognition is there that we're still doing important work for our patients and you don't necessarily need that video signal to be able to do this, and we certainly don't want to create any artificial barriers to access to care," Dr. Han said. Prior to COVID-19, telehealth services use was low because patients did not think of it as a legitimate option, but the marketplace will demand these services moving forward now that they are seeing the benefits. "I think it's important as we go ahead in the next phase ... we use the lessons we've learned during this pandemic of just large numbers of people utilizing teledermatology services to help map out what makes sense for our specialty ... as well as technical requirements that we should be asking of our vendors providing these services," Dr. Han advised. Beyond the parameters of the COVID-19 pandemic, teledermatology also provides access to care for patients in parts of the country with limited access to dermatologists, such as in rural areas. Dermatologists can use telehealth services for short hands-off visits, such as to counsel patients, check in before titrating doses, or follow-up after a cosmetic procedure. "Those are situations where you actually might improve your show rate by offering telemedicine services," Dr. Han noted. A tip sheet is available online • that provides information to help dermatologists adopt telehealth in their practice. It describes what you need, how to select a software platform, and how to monitor workflow. Patients should be asked to provide high-quality photographs before the visit via a HIPAA-secured chat or email. "We always recommend that you get a HIPAA-secured email server account if you can if you're asking for patients to send in photos, because what happens is that once they send those photos to you, you are responsible for the safety and security of that photo," Dr. Han explains. Set expectations for patients up front and be realistic about what you think is reasonable for implementing telehealth services in your practice. "If you're not comfortable seeing concerning lesions, suspicious moles, those things, you should make it very clear to your schedulers that patients should be told that if it is one of those problems, they cannot be seen by this methodology," Dr. Han recommended. * * * Hosts: Nick Andrews; Candrice R. Heath, MD (Temple University Hospital, Philadelphia) Guest: George Z. Han, MD, PhD (Icahn School of Medicine, New York) Disclosures: Dr. Heath and Dr. Han report no conflicts of interest. Show notes by: Alicia Sonners, Melissa Sears * * * You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
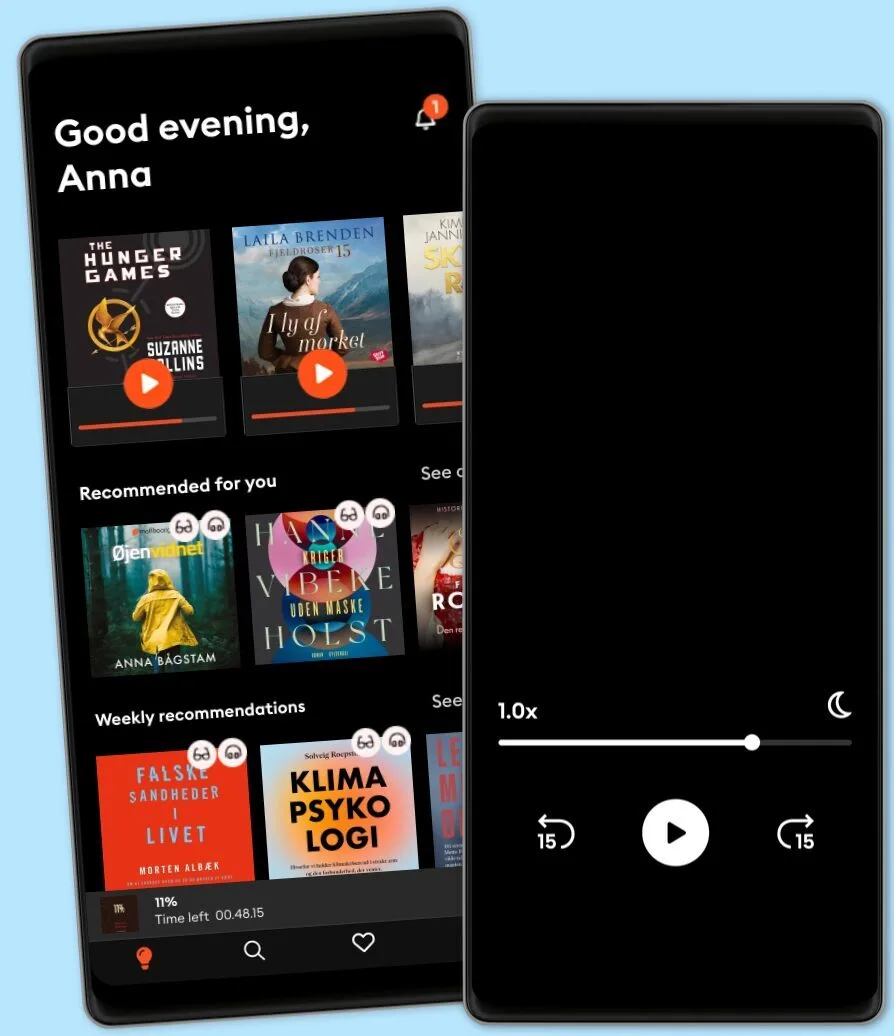
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Gabriella Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTTMIK
Dansk
Danmark