Eye complications in patients with atopic dermatitis; indoor tanning’s SCC risk; and checkpoint inhibitor combo boosts melanoma survival
- Af
- Episode
- 18
- Published
- 10. okt. 2019
- Forlag
- 0 Anmeldelser
- 0
- Episode
- 18 of 100
- Længde
- 22M
- Sprog
- Engelsk
- Format
- Kategori
- Personlig udvikling
Atopic dermatitis (AD) is associated with various ocular comorbidities that can result in permanent vision loss if left untreated. Dr. Soo Jung Kim talks with Dr. Vincent DeLeo about the incidence of keratoconjunctivitis, keratoconus, glaucoma, retinal detachment, and other ocular conditions associated with AD. Dr. Kim offers tips on spotting these complications and managing them but also indicates when referral to an ophthalmologist is necessary. We also bring you the latest in dermatology news and research. 1. Nivolumab-ipilimumab nets long-term survival in advanced melanoma An update of CheckMate 067 finds that with combination nivolumab and ipilimumab therapy, 52% of patients were alive at 5 years. 2. Lifetime indoor tanning raises risk of cutaneous squamous cell carcinoma Researchers found a dose-response association between number of indoor tanning sessions and SCC risk in Norwegian women. 3. FDA approves afamelanotide for treatment of rare condition with light-induced pain This is the first treatment approved to help patients with erythropoietic protoporphyria increase their exposure to light. * * * Things you will learn in this episode: • Patients with AD may develop blepharitis, presenting with itching and irritation of the eyelids, as well as tearing, foreign body sensations, and even photophobia. The mainstay treatment of blepharitis is good eyelid hygiene with the use of warm compresses and gentle scrubbing of the lid margins. • About 25%-52% of patients with AD have atopic keratoconjunctivitis. Clinicians should look out for red conjunctivae, hyperemia, and papillary hypertrophy of the conjunctivae. “Ultimately, if this is not treated in a timely manner, patients could have visual impairment,” explains Dr. Kim. • Keratoconus is the progressive thinning and bulging of the cornea that can affect the cornea’s topography. “Patients experience imaging blurring as well as imaging distortions,” Dr. Kim describes. “We’re not exactly sure why atopic dermatitis patients develop more keratoconus, but it’s been believed that chronic, habitual eye rubbing is most likely to be the cause due to the periocular itching.” • “Glaucoma is not necessarily a complication of atopic dermatitis; it’s more a complication of the steroid use,” explains Dr. Kim. Glaucoma in AD may be asymptomatic until advanced stages; therefore, clinicians should regularly screen patients who have a prolonged history of topical steroid application around the eye area, a family history of glaucoma, or a history of other ocular problems. • Cataracts occur in 8%-25% of patients with AD, usually younger adults. Interior or posterior subcapsular cataracts are more common in these patients compared to nuclear and cortical cataracts, which are more common in the general population. • Routine periodic screening by an ophthalmologist is required when patients have onset of periorbital atopic dermatitis, prolonged use of topical or systemic steroids, or a family history of cataracts. • The incidence of retinal detachment is 4%-8% in patients with AD. “This is a lot higher than the general population, which is around 0.005%,” Dr. Kim says. “This retinal detachment occurs usually more bilaterally at a younger age, compared to cases without atopic dermatitis.” These patients should be quickly referred to an ophthalmologist for surgical repair. • Patients with AD are at greater risk for herpetic ocular disease, and active ocular herpetic infections require urgent referral to an ophthalmologist. • Dupilumab has been associated with ocular complications in patients with AD. Host: Vincent DeLeo, MD Guest: Soo Jung Kim, MD, PhD (Baylor College of Medicine, Houston, Texas) Show notes by: Jason Orszt, Melissa Sears, Elizabeth Mechcatie You can find more of our podcasts at http://www.mdedge.com/podcasts Email the show: podcasts@mdedge.com Interact with us on Twitter: @MDedgeDerm
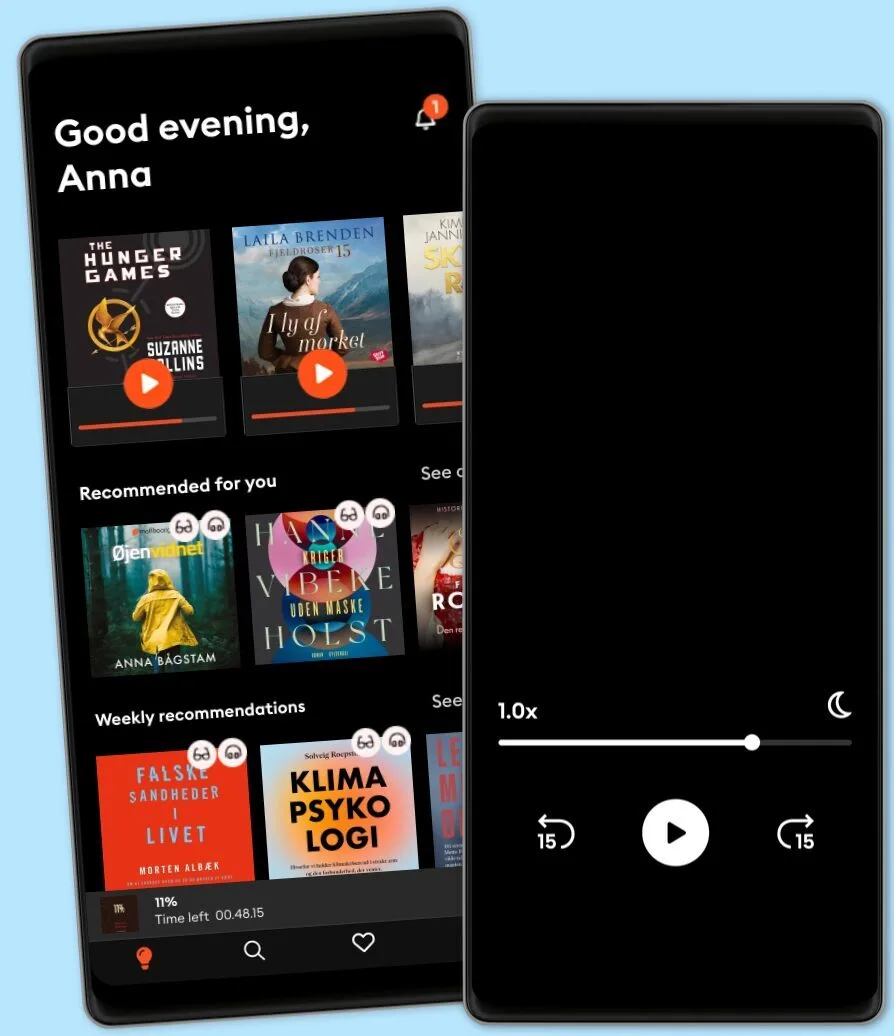
Lyt når som helst, hvor som helst
Nyd den ubegrænsede adgang til tusindvis af spændende e- og lydbøger - helt gratis
- Lyt og læs så meget du har lyst til
- Opdag et kæmpe bibliotek fyldt med fortællinger
- Eksklusive titler + Mofibo Originals
- Opsig når som helst
Other podcasts you might like ...
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTalk To Me In Korean
- Ask a ScientistScience Journal for Kids
- Story Of LanguagesSnovel Creations
- Rise With ZubinRise With Zubin
- Quint Fit EpisodesQuint Fit
- 'I AM THAT' by Ekta BathijaEkta Bathija
- Eat Smart With AvantiiAvantii Deshpande
- Intrecci - L’arte delle relazioni Ameya Canovi
- Chillin' with ICECloud10
- Minimal-ish: Minimalism, Intentional Living, MotherhoodCloud10
- Talk To Me In KoreanTalk To Me In Korean
Dansk
Danmark